Ron Bialek and John W. Moran
“Alone we can do so little; together we can do so much” ― Helen Keller1
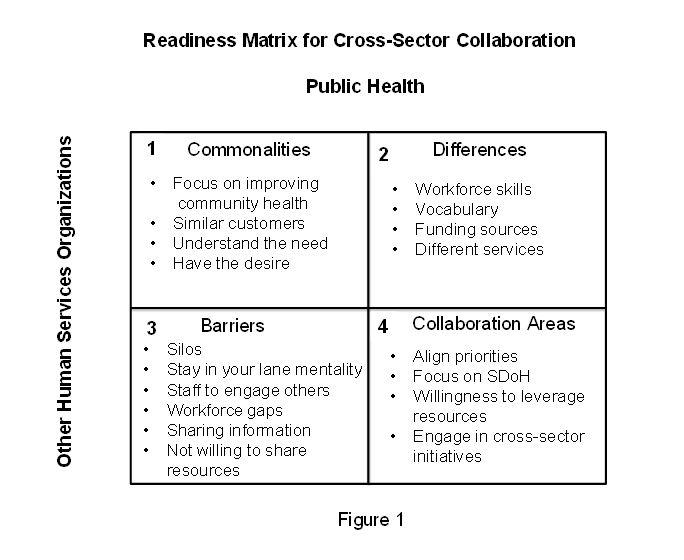
Improving a community’s health requires that the community’s public health department, healthcare institutions, and other community stakeholders providing health and health-related services break out of their comfort silo zones and work collaboratively. One of the first things a cross-sector collaborative can benefit from doing is a readiness assessment. This assessment can help gauge whether or not the various stakeholders are ready and prepared to become a successful and effective cross-sector collaborative. The Readiness Matrix for Cross-Sector Collaboration shown in Figure 1 is a structured process to help guide discussion of collaborative members about what they have in common, their differences, the barriers holding them back from collaboration, and what it will take for them to collaborate successfully. This matrix is a way to capture the responses of collaborative members. Once responses are stated, recorded, and discussed, the cross-sector collaborative should determine if it can move forward or if the barriers and differences among them are too great to overcome. If a decision is made to move forward, the collaborative should address the barriers and differences first and see how they can be resolved before taking on a community health improvement initiative. If the collaborative does not address the barriers and differences up front, these barriers and differences will more than likely surface as the collaborative tries to work on a community health issue and, at one point, derail the effort with organizations retreating back into their protective silos. The result is that an effective cross-sector collaborative will not have been developed.
To breakout of the comfort silo zones requires building true cross-sector collaboratives that work effectively and efficiently in addressing and improving specific community health issues. No one cross-sector collaborative can impact an entire community’s health, but it can focus on top priority issues. To do this, we must involve more community stakeholders, combine and share resources, offer new or improved existing services, and involve those who influence and support programs and services impacting health.
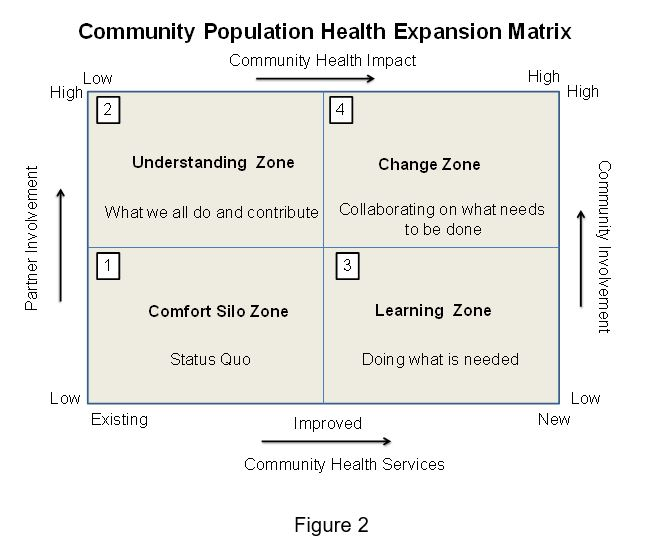
The Community Population Health Expansion Matrix shown in Figure 2 details the steps that need to be taken to breakout of the cycle of comfort silo zones once the cross-sector collaborative is formed and focused on a community health issue.
Quadrant 1 is the current state comfort silo zone. Community organizations in this quadrant are in their own lane or silo providing multiple services to the community that are not coordinated and in some cases are duplicative services. Each organization has its own perspective and voice of what is important health wise for the community. Often these voices are at odds with each other and the community hears many different messages from different stakeholders telling them “this is what is important to improve the health of the community.”
Sometimes these different voices are shaped by grants organizations receive that focus on one specific health aspect of a community such as heart disease, diabetes, smoking cessation, or opioid addiction. Once the grant goes away the voice ceases to exist and the community never hears why it ended – was the health issue resolved or the disease cured? With many voices with multiple messages, after a while the community stops listening. Also the messages may not be delivered in media that the community uses on a regular basis and the messages never get heard or are partially heard.
To breakout of this comfort silo zone requires answers to the following questions:
- Do we realize we cannot do it alone?
- Can we effectively collaborate and do it together?
- If we agree that we can collaborate, can we develop one voice for community health?
Quadrant 2 is where organizations often take initial steps outside of their silos and begin to expand their knowledge of what is going on in the community, and what other community organizations offer. To create the environment for this to happen, it is useful to develop an inventory of current services being offered by community organizations that address a particular health issue. This inventory is called “What Is In My Backyard?” The inventory provides a comprehensive overview of what the current service network consists of to help a community identify what already is in place to improve health. The inventory helps a collaborative see where the overlaps are, where the gaps are that need to be closed, and where improvements can be made.
The Community Stakeholder Services Map takes this a step further by providing a visual of the physical locations of community services in relationship to each other. This visual makes the service network come to life. It provides a way to see what a person in the community may need to do to navigate and access various community services. This helps broaden the collaborative’s view of improvements to be made to include transportation, accessibility, and safety issues for those needing the services being offered. It is a good idea for the collaborative to review the map yearly and consider shifts in demographics or other changes that may impact where the services are and should be located.
Once this is completed the following questions need to be asked:
- Are needed community services readily available and accessible?
- What community services are duplicative?
- What community services are missing?
- What are the major obstacles community residents face in order to access needed services?
Quadrant 3 is where the collaborative gains insight into how effective individual services and approaches have been in improving the community’s health, and what gaps need to be closed. This is where organizations must be willing to share their metrics and objectively analyze the data. This is where the collaborative moves from data insight to understanding the additional actions that are needed to improve the community’s health.
At this stage, it is necessary for the collaborative to answer the following questions:
- What are the community health trends and are they linear or cyclical?
- What are the contributing factors causing the data to go in its current direction?
- What are the limiting factors preventing trends from going in the right direction?
- Based on the data what must the collaborative and its members continue doing, improve, start doing, or stop doing?
Quadrant 4 is where the collaborative begins to make changes in what services are offered, and how and where these services are delivered. This is a time when it would be useful for the collaborative to develop a Population Health Driver Diagram to determine what should be done in the community to improve health. A Population Health Driver Diagram identifies primary and secondary drivers of an identified community health improvement objective and serves as a framework for determining and aligning actions that can be taken within a community for achieving improved health. This framework offers not only a starting point for discussion but also flexibility for identifying and addressing unique community characteristics, assets, and needs. It helps create an atmosphere of cooperation by enabling each participant, working to address the specific community health objective, the opportunity to identify and articulate roles already being played by that individual organization and develop an understanding of how what the organization is doing fits in with other community organizations. In addition, this framework can be used to determine other actions that can be taken individually and collectively to positively impact the particular community health objective.
To achieve successful and comprehensive collaborative action, it is important for the collaborative to answer “Yes” to the following questions:
- Are collaborative member organizations willing to collaborate, cooperate, and coordinate resources for the collective good of the community?
- Can the collaborative agree on a common health improvement AIM for the community?
- Can member organizations work collaboratively to achieve the community health improvement AIM?
- Are member organizations willing to pool and leverage assets?
- Are member organizations willing to consolidate programs and services to make them more efficient, effective, and available to achieve the community health improvement AIM?
- Are member organizations willing to allow community residents to serve on collaborative task forces?
- Are member organizations willing and prepared to allow community residents to shape the voice of health for their community?
Summary: Addressing and improving priority community health issues requires cross-sector stakeholders to collaborate, coordinate, cooperate, and co-exist in the community. It is imperative for stakeholders to work together to optimize all of the resources for the good of the community and not just for a single community organization, thus putting the “unity” back in community.